Text A Reduction: A clinician can achieve a reduction by closed manipulation – in which the displaced bone fragments are pulled into their anatomical position – restoring alignment or by open reduction through a surgical incision. Immobilisation can be achieved by internal or external fixation devices, which are available in many forms. Internal fixation involves the patient undergoing a surgical procedure and includes devices such as intramedullary nails, compression nails, plates and screws. Internal fixation is used in certain pathological fractures, when sufficient reduction cannot be maintained by external fixation, for example, when fractures involve joint surfaces, when it is important to allow early limb or joint movement, or when trying to avoid long periods of immobilisation in bed. External fixation can be achieved through surgical, as well as conservative techniques, and includes slings, cast immobilisation, skin or skeletal traction and external fixator frames.
TEXT B: Rehabilitation: Restoration of the upright position and early mobilization decrease cardiopulmonary and other immobility associated complications, for example. pressure ulcers, constipation. and urinary stasis. Following recovery or once the fracture is stable, the limb can be mobilised and range of movement exercises can begin. Deciding on the right time to begin physiotherapy is difficult. Rehabilitation should not commence too early as this may result in malunion of the bone, however, it should not even begin too late resulting in a perfect union of bone, but muscles are unable to operate the limb. Nurses have a responsibility to know what type of rehabilitation programme patients are undergoing; whether this is fully weight-bearing, partial weight-bearing, touch-toe-bearing or non-weightbearing; and also what mobilisation aids, if any, are being used, so that they are able to continue mobilising patients when physiotherapy services are not available.
Text C The complications associated with fractures can be classified as immediate, early or late. Nurses must observe for complications and take preventive measures.
| Immediate | Early | Late |
| Soft tissue damage Nerve injury Haemorrhage | Infection Neurovascular compromise Fat embolism Pulmonary embolism Deep vein thrombosis (DVT) Compartment syndrome Pressure ulcers Chest infection Exacerbation of generalised illness | Mal-union Delayed union Non-union Osteoarthritis Avascular necrosis |
Text D: Pain assessment and management: Although pain is a useful sensation in alerting us to disease or injury, it should not be accepted as a normal and inevitable part of recovery from injury or surgery. Assessment of pain is essential to ensure that the correct analgesic for the condition is prescribed and administered, and that it is having the desired effect with minimal side effects. The nurse caring for the patient, who has sustained a fracture should have knowledge of available medications and their actions, side effects and dosages. Pre-emptive analgesia should be provided so that the patient’s pain is sufficiently managed before and during rehabilitation sessions. Non-pharmacological methods of pain control such as positioning, distraction techniques and massage may also benefit patients.
In which text can you find information about:
1. Necessary to take preventive measures
2 To help the patient cope with disability.
3. Minimising the risk of deficit and in detecting early signs of the development.
4 At risk of death from a relatively simple transverse fracture of the tibia, if it is not detected.
5. To restore normal alignment of the bone.
6 To ensure that the reduced position is maintained until the bone union takes place.
7. Internal and external haemorrhage.
Questions 8-14 Answer each of the questions, 8-14, with a word or short phrase from one of the texts.
8. What can be provided for effective pain management?
9. When can it be possible to make the patient ready for movement?
10. What should not be regarded as the unavoidable part of recovery from injury?
11 What is the example given for a non-rigid method of support?
12. What may involve a surgical process?
13 What knowledge shall a nurse have when it comes to effective caring for the patient who is fractured?
14 How can reduction successfully be performed?
Questions 15-20Complete each of the sentences, 15-20, with a word or short phrase from one of the texts.
15. Because of a period of immobilisation and the effects of surgery, patients are at a risk of developing ______________
16. A ______________ may lead to osteoarthritis as a result of an abnormal distribution of load leading to an early degenerative change.
17. There are ______________ that carry the risk of damage to particular arteries.
18. Pain is considered a ______________ which make one aware of the injury.
19. A ______________ is an uncommon but serious complication.
20. Besides the blood loss from the ______________ , the sharp bone ends found in a spiral or comminuted fracture, for example, may damage the surrounding muscle or blood vessels.
PART B. For questions 1-6, choose the answer (A, B or C) which you think fits best according to the text.
1 The following is a model
A. Manual calibration B. True gravity calibration C. Wall sphygmomanometer
Mercury-gravity Manometer: The mercury-gravity manometer consists of a calibrated cartridge glass tube that is optically clear, easy to clean, and abrasion resistant. The mercury reservoir at the bottom of the tube communicates with a compression cuff through a rubber tube. When air pressure is exerted on the mercury in the reservoir by pumping the pressure bulb, the mercury in the glass tube rises and indicates how much pressure the cuff applies against the artery. The manometer is connected to the wall for ease of accurate visualization.
2 The manual gives information about;
A. Indications of emergency treatment.
B. How the device can effectively be used?
C. Indications for using the Power heart AED G3
Automatic devices like Power heart AED are intended to be used by the personnel who are trained in its operation. The user should be qualified by training in basic life support or other emergency medical response authorized by physicians. The device is indicated for emergency treatment of victims exhibiting symptoms of sudden cardiac arrest, who are unresponsive and not breathing.
Post-resuscitation, if the victim is breathing, the AED should be left attached to allow for acquisition and detection of the ECG rhythm. If a shockable ventricular tachyarrhythmia recurs, the device will charge automatically and advise the operator to deliver therapy (G3) or automatically deliver the shock (G3 Automatic). If the patient is a child or an infant up to 8 years of age, or up to 55 lbs (25kg), the device should be used with the Model 9730 Pediatric Attenuated Defibrillation Electrodes. The therapy should not be delayed to determine the exact age or weight of the patient.
3. Pick the correct statement;
A. Data suggests that NAFLD is more common than any other diseases.
B. NAFLD is more prevalent in Middle East.
C. NAFLD is more prevalent in Africa.
Prevalence of NAFLD – In Contrast to Other Diseases: The meta-analysis estimated that the overall global prevalence of NAFLD diagnosed by imaging I around 25.24% (95% CI, 22.10-28.65). The ubiquity rate of NAFLD in the Middle East can be reported as follows: (31.79% [95% CI, 13.48- 58.23]) and South America (30.45% [95% CI, 22.74-39.440]), whereas the lowest prevalence rate is reported from Africa (13.48% [5.69- 28.69]).
4 The manual talks about;
A. Critical Illness & Treatment Of Delirium
B. Delirium In Critical Care
C. Impact Of Delirium On ICU Patient
Delirium: The study of disease transmission of Delirium in sick patients is currently perceived as a general well-being issue, influencing the mechanically ventilated grown-up ICU patients up to 80%, and costing $4 to $16 billion every year in the United States alone. Effect of Delirium, as a sign of intense cerebrum brokenness, is a free critical indicator of negative clinical results in ICU patients that includes expanded mortality, healing facility LOS, expense of consideration, and long-haul psychological weakness reliable with a dementia-like state. Patients with long-haul presentation to high-measurements sedatives or medications may create physiologic reliance, and unexpected suspension may bring about medication withdrawal side effects. This session likewise incorporates Impact of Delirium on ICU Patient Outcomes, Epidemiology of insanity in ICU patients, Preventing, Detecting, and Treatment because of Alcohol and drug Withdrawal. Critical illness and appraisal of incoherence, Risk element of wooziness.
5 As per the report, what is correct?
A. Talk about 2050 neonates.
B. Major reason for admission into hospital was related to CMV.
C. Gestational age is taken as an important factor for the study conducted.
A Report; Two hundred and sixty-one neonates born at the hospital were admitted to the neonatal ICU during the study period. Two patients were excluded because they had received transfusions of blood products before urine collection (0.76%), two because the consent was not obtained (0.76%), one because the urine sample was lost (0.38%), two died before collection (0.76%) and four were lost because they were discharged early, before urine collection (1.5%).
The study population comprised 145 male NB (58%) and 105 female NB (42%).
The principal causes of admission to the ICU were prematurity (111 cases, 44.4%), respiratory dysfunction (64 cases, 25.6%), sepsis (31 cases, 12.4%) and hypoglycemia (21 cases, 8.4%). The mean weight of the newborn population studied was 2,412±900 g and mean gestational age was 35.7±3.7 weeks.
6. From the given manual, it is clear that;
A. The device will analyze ECG and can make shock deliverance simple.
B. Non-committed shock is possible through the device.
C. The device automatically shifts from one phase to other phase of operations as per the rhythmic changes.
After the AED advises a shock, it continues to monitor the ECG rhythm of the patient. If the ECG rhythm changes to a non-shockable rhythm before the actual shock is delivered, the AED will advise that the rhythm has changed and issue the prompt “RHYTHM CHANGED. SHOCK CANCELLED.” The AED will override the charge and continue ECG analysis. Synchronized Shock:- The AED is designed to automatically attempt to synchronize shock delivery on the R-wave, if one is present. If delivery cannot be synchronized within one second, a nonsynchronized shock will be delivered.
PART C. TEXT 1. OPIOID-INDUCED CONSTIPATION
The human opioid system is highly complex and includes three main endogenous opioid receptors (µ, κ and δ receptors), as well as a number of endogenous opioid peptides such as endorphins, enkephalins, and dynorphins, which activate these receptors. Opioid receptors are widely distributed in the brain and spinal cord, as well as in a variety of peripheral tissues such as the gut, airways, blood vessels, and heart. When activated, the opioid receptors located in the brain and spinal cord mediate the analgesic effects of the opioids. Unfortunately, activation of opioid receptors in the gut can significantly impair intestinal activity and lead to OIC.
Mu-opioid receptors, and to a lesser extent κ-opioid receptors, are expressed extensively throughout the gastrointestinal tract and enteric nervous system. When opioid receptors are stimulated they may alter or more precisely decrease peristalsis, inhibit intestinal transit, increase intestinal fluid absorption and decrease intestinal secretions. All of these effects combine to cause significant constipation. A clinical syndrome of opioid-induced bowel dysfunction may occur with chronic opioid use that is characterized by abdominal pain, hard stools, fecal impaction, anorexia, nausea and vomiting.
A 2009 study by Bell et al., examined the prevalence, severity and impact of OIC in 322 patients taking daily opioids. The investigators found that 81% of the patients in their study reported OIC and that the majority of patients with OIC reported at least a moderate negative impact on quality of life and activities of daily living. One third of patients with OIC missed the doses, decreased dosage or stopped using opioids completely in order to improve their bowel function. A second study by Bell found that the patients with OIC were more likely to take time off from work and were less productive in both their work and home environments.
With continued opioid use, patients often become adept at dealing with the analgesic effects of the opioids. The mechanism of opioid tolerance is likely related to down-regulation (decreased numbers) or desensitization of µ-opioid receptors in the CNS. Binding of opioids to the µ receptor activates numerous downstream intracellular pathways. Activated G-protein-dependent signaling pathways appear involved in receptor desensitization while G-proteinin dependent signaling pathways appear to facilitate µ receptor endocytosis and subsequent downregulation of receptors. Fortunately, tolerance to the respiratory depressant effects of the opioids also develops in parallel to the tolerance seen with the analgesic effects. Interestingly, however, tolerance does not occur to the constipating effect of the opioids.
Opioid-induced constipation and opioid bowel dysfunction presents with a myriad of symptoms. Diagnosis of OIC should begin with a detailed patient history that includes frequency of bowel movements, the consistency of stool, and the presence of straining, pain, nausea and vomiting. A physical examination should also be conducted including the bowel sounds, and abdominal palpation for firmness, distention and the presence of pain. The possibility of fecal impaction should also be assessed in patients with persistent and severe constipation. A number of nonpharmacologic and pharmacologic options are available with respect to effective elimination of this condition. Although current treatment recommendations support the prophylactic use of various bowel regimens in patients receiving opioid therapy, definitive studies showing the superiority of one treatment regimen over another are currently lacking.
The overall strategy to prevent OIC and to start with the onset of opioid therapy, include adequate fluid and fiber intake, and increased physical activity. A recent study showed that patients with post- operative constipation, who received bowel massage by nurses had reduced symptoms of constipation, increased stool output and improved quality of life with no significant adverse side effects. However, in another study, it is showed that while abdominal massage was useful for decreasing the severity of constipation symptoms, it did not lead to curtailing down of laxative. Bowel “diaries” which track the frequency of bowel movements might also be helpful for determining the severity of the OIC that is occurring. While helpful, nonpharmacologic interventions are seldom successful alone for the management of OIC.
Senior nurses should be ideally situated to identify patients at high risk for OIC and ruling out other causes of chronic constipation. A detailed patient history should be obtained, which will include physical activity, and a review of all medications the patient is currently taking. A thorough patient examination should be conducted and accompanying signs and symptoms such nausea, vomiting or abdominal pain/distention should be noted. Nurses should monitor patient bowel habits as well as the quantity and quality of stools.
7. In the first paragraph, the writer talks about;
A. OIC in general
B. Types of OIC receptors
C. How OIC occurs?
D. Distribution of opioid receptors.
8. As per paragraph two, activation of opioid receptors will;
A. Lead to intestinal movement
B. Cause hard stools
C. Lead to constipation
D. Cause abdominal pain
9. What do we learn about OIC in the third paragraph?
A. Research conducted by Bell
B. Impact of OIC on life
C. How OIC will affect?
D. Cessation of opioid pain therapy
10 What do we learn from the fourth paragraph?
A. Opioid acceptance behaviour among patients
B. Ability to deal with the analgesic effects
C. Resilience and OIC
D. Opioid Tolerance and OIC
11. What is not right as per the information given in the fifth paragraph?
A. A large number of symptoms arises that lead to OIC.
B. Detection of bowel sounds, presence of nausea are common.
C. Patients suffering from the disease will vomit, feel abdominal pain.
D. None of the above
12. In paragraph six, the writer gives information on;
A. How OIC can easily be avoided?
B. Nonpharmacologic management of OIC.
C. Steps to be taken to deal with OIC.
D. How OIC can be prevented?
13. Pick the incorrect statement related to the study performed as explained by the writer;
A. Only nonpharmacologic interventions can be effective.
B. Bowel massage is effective in eliminating many of the problems associated with OIC.
C. Stool output can be improved.
D. Use of laxative can certainly be decreased.
14 In the final paragraph, the writer talks about;
A. Importance of taking patient`s history.
B. Identifying risks.
C. Role of the advanced practice nurse in OIC.
D. Treatment procedure.
PART C. TEXT 2: VACCINATION
Vaccination as a deliberate attempt to protect human beings against disease has a long history and more widespread use of vaccines could prevent about 1.6 million deaths a year among children less than five years of age. Over the next few years a new generation of vaccines will become available that could save the lives of up to 10 million individuals: e.g., vaccines against diarrhoeal diseases, hepatitis C, malaria, acquired immunodeficiency syndrome (AIDS), sexually transmitted and other diseases. Current development efforts seek combination vaccines that protect against multiple pathogens, with a goal of combining all the antigens recommended for routine immunization into a single multivalent product.
Combining multiple related or unrelated antigens into a single vaccine is not a new concept and the first combination vaccine licensed in the United States of America was trivalent influenza in 1945. Diphtheria, Pertussis, Tetanus (DPT) vaccine although developed in 1943, was not licensed till 1948. Efforts to overcome the interference seen with simultaneous administration of three live vaccines delayed the licensing of trivalent Oral Polio Vaccine (OPV) till 1963. Measles, Mumps,Rubella (MMR) was licensed in 1971 and quadrivalent meningococcal vaccine in 1978.
Combining multiple antigens into one injection requires demonstration that the combination will not materially reduce the safety or immunogenicity of the component vaccines. Combination vaccine trials should be prospective, randomised, double blinded and should have control (comparison) groups.Identifying the control groups could be problematic when multicomponent vaccine is evaluated. Other factors like sequence of administration of certain antigens may play an important role in immunogenicity.
The interaction can enhance the immune response to individual components as it occurs in whole cell pertussis vaccine, when combined with diphtheria toxoid. Usually, a combination of vaccines results in no effect or a depression of immune response to one or more vaccine component. It is an immunologic phenomenon relevant to combination vaccines, antibody responses to hapten polysaccharide vaccine (e.g. H influenzae b) presented on a carrier protein (e.g. tetanus toxoid,diphtheria toxoid) are inhibited by prior immunization with the specific carrier.Combination live vaccines can interfere immunologically with each other, e.g., one vaccine may stimulate interferon production that may inhibit replication of another virus.
Interest in combining DPT/IPV was generated when enhanced potency IPV became available, thus eliminating the necessity of frozen shipments for OPV. In addition, administration of IPV would eliminate the risk of vaccine-associated polio. Antibody responses to pertussis and poliovirus components may be substantially reduced in combination than when given alone. However, poliovirus seroconversion rates and absolute antibody levels remained high in combined vaccines. Various studies have compared DPT combinations with unconjugated Polyribose phosphate (PRP) or conjugated PRP Hib vaccine. A number of studies have evaluated these combination vaccines and results are variable. In general, the groups with lower antibody responses still attained levels considered protective. One study evaluated the effect of booster dose of DPT/Hepatitis B/Hib given to subjects, who received DPT/Hepatitis B/ Hib for the primary series. The group hadhigh antibody response and mean levels were higher in the group primed with DPT/Hepatitis B/Hib, especially with PRP (Hib).
DTaP/HB combination vaccine retains the immunogenicity and safety profiles of the separate components and delivers good antibody concentrations at a variety of schedules. A comparison of combination vaccine at 2, 4, 6 months versus the currently recommended schedules-HB at birth, 1 & 6 months and DPT at 6, 10 & 14 weeks, found similar or higher antibody responses for combined vaccine for every component, which was significantly lower. However, the mean HB antibody levels were high and 98% of subjects had levels greater than 10mIU/mL, which are considered protective. A study comparing combination vaccine and separate vaccines given at 2, 4, 6 and booster between 12 and 15 months of age has shown that the antibody response to Hib, were 72% and 76% at 6 months, increasing to 92% and 93% after booster dose with combination and separate vaccines respectively.
15. In the first paragraph, writer says that;
A. Combination vaccines are the new phase of development.
B. Vaccines implemented have changed lives of people across the globe.
C. Vaccines provide effective protection from a large number of pathogens c.
D. Use of vaccines have led to curtailing down of deaths in millions.
16. In paragraph 2, the writer says
A. Combination vaccines came into being in 1940s.
B. DPT was the first combined vaccine to be used.
C. OPV was not introduced before 1963.
D. MMR is an example of effective combined vaccine.
17. Paragraph three talks about;
A. Immunogenicity of the prepared vaccines.
B. Importance of conducting trails.
C. Facts that have direct impact on immunogenicity.
D. Challenges in the development of combined vaccines.
18 In paragraph four, the writer has described;
A. Immunological interference
B. Antigen role
C. Induction of interferon
D. B and C
19. Immunologic phenomena relevant to combination vaccines gives an idea about;
A. Induction of interferon B.
Carrier induced epitope expression
C. Antigen competition
D. Immunological interference
20 As per paragraph five, what is more relevant?
A. DPT/Conjugate (Hib) will often be not more effective.
B. Combined vaccines often produce different results.
C. DPT/IPV came into being only after potency IPV became available.
D. DPT/Hepatitis B and DPT/Hepatitis B/Hib have more potential to produce same results
21. In paragraph 6, the writer says;
A. Taking vaccines at an early age is important.
B. Various combinations bring in various results.
C. Combinations with DTaP is proven to be more effective
D. Separate vaccine shall be given as needed
22 In final paragraph, writer has directly or indirectly implied that;
A. Vaccines for newborn and children less than 3 years old are known to be more powerful.
B. Combined vaccines may not be as effective as separate vaccines.
C. Separate vaccines are more effective than combined vaccines.
D. Combined vaccine helps with retaining immunogenicity.
How did it go? Please share your feedback in the comment section below:
VIEW ANSWER KEYSOET READINGOET SPEAKINGOET ROLE PLAYSOET LETTER WRITINGOET LISTENINGFree admission and English Courses. കാശ് കൊടുക്കാതെ അഡ്മിഷൻ. FREE ഇഗ്ലീഷ് കോഴ്സുകൾ. ഈ ഓഫർ നേടൂ. Contact us at +91 9886926773 പ്രോസസ്സിംഗ് ആയാസകരം.

New batch is open. Join today!
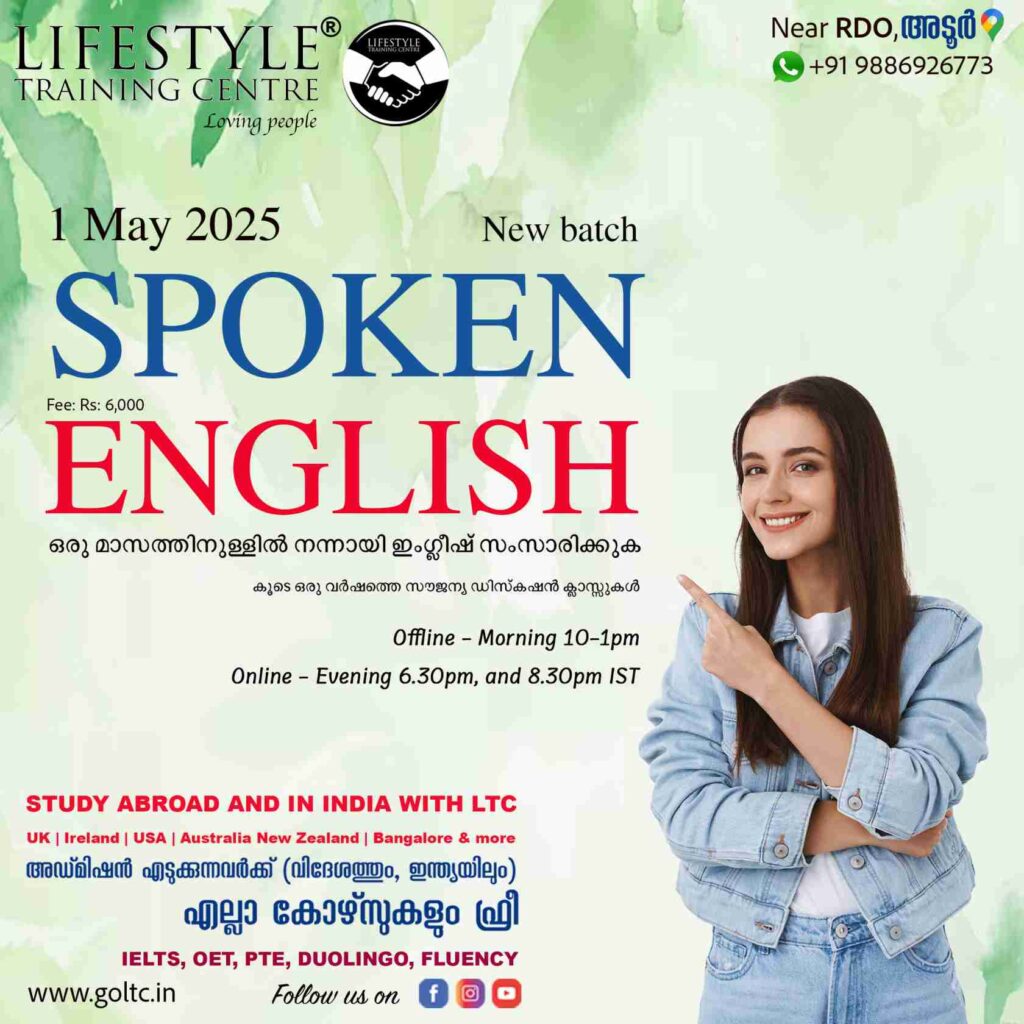
Ready to study abroad or master OET, PTE, IELTS, Duolingo, Phonetics, or Spoken English?
📞 Call us now at +91 9886926773
📱 Call/WhatsApp/Text: +91 9886926773
📧 Email: [email protected]
Visit us in person by following the directions on Google Maps. We look forward to welcoming you to the Lifestyle Training Centre.
Follow Lifestyle Training Centre on social media:
Thank you very much!
Would you like to download a copy of the practice test? Please click on the download button below:


Pingback: TREATMENT OF FRACTURES OET READING | Lifestyle Training Centre®