TEXT A: Paracetamol: contraindications and interactions
4.4 Special warnings and precautions for use
Where analgesics are used long-term (>3 months) with administration every two days or more frequently, headache may develop or increase. Headache induced by overuse of analgesics (MOH medication-overuse headache) should not be treated by dose increase. In such cases, the use of analgesics should be discontinued in consultation with the doctor.
Care is advised in the administration of paracetamol to patients with alcohol dependency, severe renal or severe hepatic impairment. Other contraindications are: shock and acute inflammation of liver due to hepatitis C virus. The hazards of overdose are greater in those with non-cirrhotic alcoholic liver disease.
4.5 Interaction with other medicinal products and other forms of interaction
• Anticoagulants – the effect of warfarin and other coumarins may be enhanced by prolonged regular use of paracetamol with increased risk of bleeding. Occasional doses have no significant effect.
• Metoclopramide – may increase speed of absorption of paracetamol.
• Domperidone – may increase speed of absorption of paracetamol.
• Colestyramine – may reduce absorption if given within one hour of paracetamol.
• Imatinib–restriction or avoidance of concomitant regular paracetamol use should be taken with imatinib.
A total of 169 drugs (1042 brand and generic names) are known to interact with paracetamol. 14 major drug interactions (e.g., amyl nitrite)
62 moderate drug interactions
93 minor drug interactions
A total of 118 brand names are known to have paracetamol in their formulation, e.g. Lemsip

Text D
Clinical Assessment
• Commonly, patients who have taken a paracetamol overdose are asymptomatic for the first 24 hours or just have nausea and vomiting
• Hepatic necrosis (elevated transaminases, right upper quadrant pain and jaundice) begins to develop after 24 hours and can progress to acute liver failure (ALF)
• Patients may also develop:
• Encephalopathy • Renal failure – usually occurs around day three
• Oliguria • Lactic acidosis
• Hypoglycaemia
History
• Number of tablets, formulation, any concomitant tablets
• Time of overdose
• Suicide risk – was a note left?
• Any alcohol taken (acute alcohol ingestion will inhibit liver enzymes and may reduce the production of the toxin NAPQI, whereas chronic alcoholism may increase it)
Questions 1-20
1 the various symptoms of patients who have taken too much paracetamol?
2 the precise levels of paracetamol in the blood which require urgent intervention?
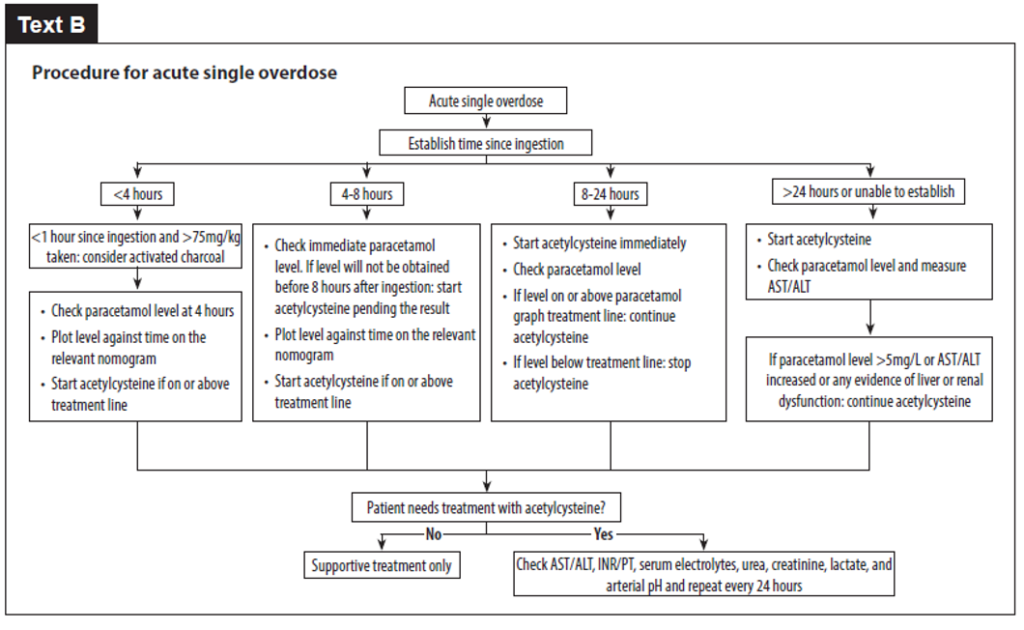
3 the steps to be taken when treating a paracetamol overdose patient?
4 whether paracetamol overdose was intentional?
5 the number of products containing paracetamol?
6 what to do if there are no details available about the time of the overdose?
7 dealing with paracetamol overdose patients who have not received adequate nutrition?
Questions 8-13. Answer each of the questions, 8-13, with a word or short phrase from one of the texts. Each answer may include words, numbers or both.
8 If paracetamol is used as a long-term painkiller, what symptom may get worse?
9 It may be dangerous to administer paracetamol to a patient with which viral condition?
10 What condition may develop in an overdose patient who presents with jaundice?
11 What condition may develop on the third day after an overdose?
12 What drug can be administered orally within 10 – 12 hours as an alternative to acetylcysteine?
13 What treatment can be used if a single overdose has occurred less than an hour ago?
Questions 14-20. Complete each of the sentences, 14-20, with a word or short phrase from one of the texts. Each answer may include words, numbers or both.
14 If a patient has taken metoclopramide alongside paracetamol, this may affect the__________ of the paracetamol.
15 After 24 hours, an overdose patient may present with pain in the .
16 For the first 24 hours after overdosing, patients may only have such symptoms as______________
17 Acetylcysteine should be administered to patients with a paracetamol level above the high-risk treatment line who are taking any type of _______________medication.
18 A non-high-risk patient should be treated for paracetamol poisoning if their paracetamol level is above_______________ mg/litre 8 hours after overdosing.
19 A high-risk patient who overdosed _________________hours ago should be given acetylcysteine if their paracetamol level is 25 mg/litre or higher.
20 If a patient does not require further acetylcysteine, they should be given treatment categorised as_____________ only.
PART B. For questions 1-6, choose the answer (A, B or C)
1. This guideline extract says that the nurse in charge
A. must supervise the opening of the controlled drug cupboard.
B should make sure that all ward cupboard keys are kept together.
C can delegate responsibility for the cupboard keys to another ward.
Medicine Cupboard Keys: The keys for the controlled drug cupboard are the responsibility of the nurse in charge. They may be passed to a registered nurse in order for them to carry out their duties and returned to the nurse in charge. If the keys for the controlled drug cupboard go missing, the locks must be changed and pharmacy informed and an incident form completed. The controlled drug cupboard keys should be kept separately from the main body of keys. Apart from in exceptional circumstances, the keys should not leave the ward or department. If necessary, the nurse in charge should arrange for the keys to be held in a neighbouring ward or department by the nurse in charge there.
2. When seeking consent for a post-mortem examination, it is necessary to
A. give a valid reason for conducting it.
B allow all relatives the opportunity to decline it.
C only raise the subject after death has occurred.
Post-Mortem Consent: A senior member of the clinical team, preferably the Consultant in charge of the care, should raise the possibility of a post-mortem examination with the most appropriate person to give consent. The person consenting will need an explanation of the reasons for the post-mortem examination and what it hopes to achieve. The first approach should be made as soon as it is apparent that a post-mortem examination may be desirable, as there is no need to wait until the patient has died. Many relatives are more prepared for the consenting procedure if they have had time to think about it beforehand.
3. The purpose of these notes about an incinerator is to
A help maximise its efficiency.
B give guidance on certain safety procedures.
C recommend a procedure for waste separation.
Low-cost incinerator: General operating notes: 3.2.1 Hospital waste management: Materials with high fuel values such as plastics, paper, card and dry textile will help maintain high incineration temperature. If possible, a good mix of waste materials should be added with each batch. This can best be achieved by having the various types of waste material loaded into separate bags at source, i.e., wards and laboratories, and clearly labelled. It is not recommended that the operator sorts and mixes waste prior to incineration as this is potentially hazardous. If possible, some plastic materials should be added with each batch of waste as this burns at high temperatures. However, care and judgement will be needed, as too much plastic will create dense dark smoke.
4. What does this manual tell us about spacer devices?
A Patients should try out a number of devices with their inhaler.
B They enable a patient to receive more of the prescribed medicine.
C Children should be given spacers which are smaller than those for adults.
Manual extract: Spacer devices for asthma patients: Spacer devices remove the need for co-ordination between actuation of a pressurized metered-dose inhaler and inhalation. In addition, the device allows more time for evaporation of the propellant so that a larger proportion of the particles can be inhaled and deposited in the lungs. Spacer devices are particularly useful for patients with poor inhalation technique, for children, for patients requiring higher doses, for nocturnal asthma, and for patients prone to candidiasis with inhaled corticosteroids. The size of the spacer is important, the larger spacers with a one-way valve being most effective. It is important to prescribe a spacer device that is compatible with the metered-dose inhaler. Spacer devices should not be regarded as interchangeable; patients should be advised not to switch between spacer devices.
5. The email is reminding staff that the
A benefits to patients of using bedrails can outweigh the dangers.
B number of bedrail-related accidents has reached unacceptable levels.
C patient’s condition should be central to any decision about the use of bedrails.
To: All Staff
Subject: Use of bed rails
Please note the following.
Patients in hospital may be at risk of falling from bed for many reasons including poor mobility, dementia or delirium, visual impairment, and the effects of treatment or medication. Bedrails can be used as safety devices intended to reduce risk. However, bedrails aren’t appropriate for all patients, and their use involves risks. National data suggests around 1,250 patients injure themselves on bedrails annually, usually scrapes and bruises to their lower legs. Statistics show 44,000 reports of patient falls from bed annually resulting in 11 deaths, while deaths due to bedrail entrapment occur less than one every two years, and are avoidable if the relevant advice is followed. Staff should continue to take great care to avoid bedrail entrapment, but be aware that in hospital settings there may be a greater risk of harm to patients who fall out of bed.
6. What does this extract from a handbook tell us about analeptic drugs?
A They may be useful for patients who are not fully responsive.
B Injections of these drugs will limit the need for physiotherapy.
C Care should be taken if they are used over an extended period.
Analeptic drugs: Respiratory stimulants (analeptic drugs) have a limited place in the treatment of ventilatory failure in patients with chronic obstructive pulmonary disease. They are effective only when given by intravenous injection or infusion and have a short duration of action. Their use has largely been replaced by ventilatory support. However, occasionally when ventilatory support is contra-indicated and in patients with hypercapnic respiratory failure who are becoming drowsy or comatose, respiratory stimulants in the short term may arouse patients sufficiently to co-operate and clear their secretions.
Respiratory stimulants can also be harmful in respiratory failure since they stimulate non-respiratory as well as respiratory muscles. They should only be given under expert supervision in hospital and must be combined with active physiotherapy. At present, there is no oral respiratory stimulant available for long- term use in chronic respiratory failure.
PART C. TEXT 1: PATIENT SAFETY. Choose the answer (A, B, C or D)
Highlighting a collaborative initiative to improve patient safety
In a well-documented case in November 2004, a female patient called Mary was admitted to a hospital in Seattle, USA, to receive treatment for a brain aneurysm. What followed was a tragedy, made worse by the fact that it needn’t have occurred at all. The patient was mistakenly injected with the antiseptic chlorhexidine. It happened, the hospital says, because of ‘confusion over the three identical stainless-steel bowls in the procedure room containing clear liquids — chlorhexidine, contrast dye and saline solution’. Doctors tried amputating one of Mary’s legs to save her life, but the damage to her organs was too great: she died 19 days later.
This and similar incidents are what inspired Professor Dixon-Woods of the University of Cambridge, UK, to set out on a mission: to improve patient safety. It is, she admits, going to be a challenge. Many different policies and approaches have been tried to date, but few with widespread success, and often with unintended consequences. Financial incentives are widely used, but recent evidence suggests that they have little effect. ‘There’s a danger that they tend to encourage effort substitution,’ explains Dixon-Woods. In other words, people concentrate on the areas that are being incentivised, but neglect other areas. ‘It’s not even necessarily conscious neglect. People have only a limited amount of time, so it’s inevitable they focus on areas that are measured and rewarded.’
In 2013, Dixon-Woods and colleagues published a study evaluating the use of surgical checklists introduced in hospitals to reduce complications and deaths during surgery. Her research found that that checklist may have little impact, and in some situations might even make things worse. ‘The checklists sometimes introduced new risks. Nurses would use the lists as box-ticking exercises – they would tick the box to say the patient had had their antibiotics when there were no antibiotics in the hospital, for example.’ They also reinforced the hierarchies– nurses had to try to get surgeons to do certain tasks, but the surgeons used the situation as an opportunity to display their power and refuse.
Dixon-Woods and her team spend time in hospitals to try to understand which systems are in place and how they are used. Not only does she find differences in approaches between hospitals, but also between units and even between shifts. ‘Standardisation and harmonisation are two of the most urgent issues we have to tackle. Imagine if you have to learn each new system wherever you go or even whenever a new senior doctor is on the ward. This introduces massive risk.’
Dixon-Woods compares the issue of patient safety to that of climate change, in the sense that it is a ‘problem of many hands’, with many actors, each making a contribution towards the outcome, and there is difficulty in identifying where the responsibility for solving the problem lies. ‘Many patient safety issues arise at the level of the system as a whole, but policies treat patient safety as an issue for each individual organisation.’
Nowhere is this more apparent than the issue of ‘alarm fatigue’, according to Dixon-Woods. Each bed in an intensive care unit typically generates 160 alarms per day, caused by machinery that is not integrated. ‘You have to assemble all the kit around an intensive care bed manually,’ she explains. ‘It doesn’t come built as one like an aircraft cockpit. This is not something a hospital can solve alone. It needs to be solved at the sector level.’
Dixon-Woods has turned to Professor Clarkson in Cambridge’s Engineering Design Centre to help. ‘Fundamentally, my work is about asking how we can make it better and what could possibly go wrong,’ explains Clarkson. ‘We need to look through the eyes of the healthcare providers to see the challenges and to understand where tools and techniques we use in engineering may be of value.’ There is a difficulty, he concedes: ‘There’s no formal language of design in healthcare. Do we understand what the need is? Do we understand what the requirements are? Can we think of a range of concepts we might use and then design a solution and test it before we put it in place? We seldom see this in healthcare, and that’s partly driven by culture and lack of training, but partly by lack of time.’ Dixon-Woods agrees that healthcare can learn much from engineers. ‘There has to be a way of getting our two sides talking,’ she says. ‘Only then will we be able to prevent tragedies like the death of Mary.’
7. What point is made about the death of a female patient called Mary?
A It was entirely preventable.
B Nobody was willing to accept the blame.
C Surgeons should have tried harder to save her life.
D It is the type of incident which is becoming increasingly common.
8. What is meant by the phrase ‘effort substitution’ in the second paragraph?
A Monetary resources are diverted unnecessarily.
B Time and energy is wasted on irrelevant matters.
C Staff focus their attention on a limited number of issues.
D People have to take on tasks which they are unfamiliar with.
9. By quoting Dixon-Woods in the second paragraph, the writer shows that the professor
A understands why healthcare employees have to make certain choices.
B doubts whether reward schemes are likely to put patients at risk.
C believes staff should be paid a bonus for achieving goals.
D feels the people in question have made poor choices.
10. What point is made about checklists in the third paragraph?
A Hospital staff sometimes forget to complete them.
B Nurses and surgeons are both reluctant to deal with them.
C They are an additional burden for over-worked nursing staff.
D The information recorded on them does not always reflect reality.
11. What problem is mentioned in the fourth paragraph?
A failure to act promptly
B outdated procedures
C poor communication
D lack of consistency
12. What point about patient safety is the writer making by quoting Dixon-Woods’ comparison with climate change?
A The problem will worsen if it isn’t dealt with soon.
B It isn’t clear who ought to be tackling the situation.
C It is hard to know what the best course of action is.
D Many people refuse to acknowledge there is a problem.
13. The writer quotes Dixon-Woods’ reference to intensive care beds in order to
A present an alternative viewpoint.
B illustrate a fundamental obstacle.
C show the drawbacks of seemingly simple solutions.
D give a detailed example of how to deal with an issue.
14. What difference between healthcare and engineering is mentioned in the final paragraph?
A the types of systems they use
B the way they exploit technology
C the nature of the difficulties they face
D the approach they take to deal with challenges
PART C. TEXT 2:
MIGRAINE – MORE THAN JUST A HEADACHE
When a news reporter in the US gave an unintelligible live TV commentary of an awards ceremony, she became an overnight internet sensation. As the paramedics attended, the worry was that she’d suffered a stroke live on air. Others wondered if she was drunk or on drugs. However, in interviews shortly after, she revealed, to general astonishment, that she’d simply been starting a migraine. The bizarre speech difficulties she experienced are an uncommon symptom of aura, the collective name for a range of neurological symptoms that may occur just before a migraine headache. Generally, aura is visual – for example blind spots which increase in size, or have a flashing, zig-zagging or sparkling margin, but they can include other odd disturbances such as pins and needles, memory changes and even partial paralysis.
Migraine is often thought of as an occasional severe headache, but surely symptoms such as these should tell us there’s more to it than meets the eye. In fact, many scientists now consider it a serious neurological disorder. One area of research into migraine aura has looked at the phenomenon known as Cortical Spreading Depression (CSD) – a storm of neural activity that passes in a wave across the brain’s surface. First seen in 1944 in the brain of a rabbit, it’s now known that CSD can be triggered when the normal flow of electric currents within and around brain cells is somehow reversed. Nouchine Hadjikhani and her team at Harvard Medical School managed to record an episode of CSD in a brain scanner during migraine aura (in a visual region that responds to flickering motion), having found a patient who had the rare ability to be able to predict when an aura would occur. This confirmed a long-suspected link between CSD and the aura that often precedes migraine pain. Hadjikhani admits, however, that other work she has done suggests that CSD may occur all over the brain, often unnoticed, and may even happen in healthy brains. If so, aura may be the result of a person’s brain being more sensitive to CSD than it should be.
Hadjikhani has also been looking at the structural and functional differences in the brains of migraine sufferers. She and her team found thickening of a region known as the somatosensory cortex, which maps our sense of touch in different parts of the body. They found the most significant changes in the region that relates to the head and face. ‘Because sufferers return to normal following an attack, migraine has always been considered an episodic problem,’ says Hadjikhani. ‘But we found that if you have successive strikes of pain in the face area, it actually increases cortical thickness.’
Work with children is also providing some startling insights. A study by migraine expert Peter Goadsby, who splits his time between King’s College London and the University of California, San Francisco, looked at the prevalence of migraine in mothers of babies with colic – the uncontrolled crying and fussiness often blamed on sensitive stomachs or reflux. He found that of 154 mothers whose babies were having a routine two-month check-up, the migraine sufferers were 2.6 times as likely to have a baby with colic. Goadsby believes it is possible that a baby with a tendency to migraine may not cope well with the barrage of sensory information they experience as their nervous system starts to mature, and the distress response could be what we call colic.
Linked to this idea, researchers are finding differences in the brain function of migraine sufferers, even between attacks. Marla Mickleborough, a vision specialist at the University of Saskatchewan in Saskatoon, Canada, found heightened sensitivity to visual stimuli in the supposedly ‘normal’ period between attacks. Usually, the brain comes to recognise something repeating over and over again as unimportant and stops noticing it, but in people with migraine, the response doesn’t diminish over time. ‘They seem to be attending to things they should be ignoring,’ she says.
Taken together this research is worrying and suggests that it’s time for doctors to treat the condition more aggressively, and to find out more about each individual’s triggers so as to stop attacks from happening. But there is a silver lining. The structural changes should not be likened to dementia, Alzheimer’s disease or ageing, where brain tissue is lost or damaged irreparably. In migraine, the brain is compensating. Even if there’s a genetic predisposition, research suggests it is the disease itself that is driving networks to an altered state. That would suggest that treatments that reduce the frequency or severity of migraine will probably be able to reverse some of the structural changes too. Treatments used to be all about reducing the immediate pain, but now it seems they might be able to achieve a great deal more.
15. Why does the writer tell the story of the news reporter?
A to explain the causes of migraine aura
B to address the fear surrounding migraine aura
C to illustrate the strange nature of migraine aura
D to clarify a misunderstanding about migraine aura
16. The research by Nouchine Hadjikhani into CSD
A has less relevance than many believe.
B did not result in a definitive conclusion.
C was complicated by technical difficulties.
D overturned years of accepted knowledge.
17. What does the word ‘This’ in the second paragraph refer to?
A the theory that connects CSD and aura
B the part of the brain where auras take place
C the simultaneous occurrence of CSD and aura
D the ability to predict when an aura would happen
18. The implication of Hadjikhani’s research into the somatosensory cortex is that
A migraine could cause a structural change.
B a lasting treatment for migraine is possible.
C some diagnoses of migraine may be wrong.
D having one migraine is likely to lead to more.
19. What does the writer find surprising about Goadsby’s research?
A the idea that migraine may not run in families
B the fact that migraine is evident in infanthood
C the link between childbirth and onset of migraine
D the suggestion that infant colic may be linked to migraine
20. According to Marla Mickleborough, what is unusual about the brain of migraine sufferers?
A It fails to filter out irrelevant details.
B It struggles to interpret visual input.
C It is slow to respond to sudden changes.
D It does not pick up on important information.
21. The writer uses the phrase ‘a silver lining’ in the final paragraph to emphasise
A the privileged position of some sufferers.
B a more positive aspect of the research.
C the way migraine affects older people.
D the value of publicising the research.
22. What does the writer suggest about the brain changes seen in migraine sufferers?
A Some of them may be beneficial.
B They are unlikely to be permanent.
C Some of them make treatment unnecessary.
D They should still be seen as a cause for concern.
How did it go? Please share your feedback in the comment section below:
Free admission and English Courses. കാശ് കൊടുക്കാതെ അഡ്മിഷൻ. FREE ഇഗ്ലീഷ് കോഴ്സുകൾ. ഈ ഓഫർ നേടൂ. Contact us at +91 9886926773 പ്രോസസ്സിംഗ് ആയാസകരം.

New batch is open. Join today!

Ready to study abroad or master OET, PTE, IELTS, Duolingo, Phonetics, or Spoken English?
📞 Call us now at +91 9886926773
📱 Call/WhatsApp/Text: +91 9886926773
📧 Email: mail@goltc.in
Visit us in person by following the directions on Google Maps. We look forward to welcoming you to the Lifestyle Training Centre.
Follow Lifestyle Training Centre on social media:
Thank you very much!
Would you like to download a copy of the practice test? Please click on the download button below:


Pingback: PARACETAMOL OVERDOSE OET READING ANSWERS | Lifestyle Training Centre®