TEXT 1 What is a ganglion cyst?
A ganglion cyst is a collection of synovial fluid in a sac, on or near tendon sheaths and joint capsules. They usually appear on the on the dorsal aspect of hands, fingers and wrists, and can also occur on the feet, ankles and knees. The cyst can range from the size of a pea to the size of a golf ball. The size of a ganglion may increase over time, especially if it near a joint where there are frequent repetitive movements.
About 65% of ganglia of the wrist and hand are dorsal wrist ganglia, followed by the volar wrist ganglion constituting about 20 to 25% of ganglia. Flexor tendon sheath ganglia and mucous cysts arising from the dorsal distal interphalangeal joint make up the remaining 10 to 15%.
Ganglion cysts look and feel like a smooth lump under the skin and the wall of the ganglion is smooth, fibrous, and of variable thickness. The cyst is filled with clear gelatinous, sticky, or mucoid fluid of high viscosity. The fluid in the cyst is sometimes almost pure hyaluronic acid. The cyst is attached to the tendon or joint by a pedicle (stalk).
The cause of them is not known, however it is thought they may be caused by tiny tears in the covering of a tendon or joint. Ganglion cysts are benign and appear in isolation. Around 30 to 50 per cent of ganglion cysts resolve spontaneously without medical intervention, though this can take many years.
Ganglia constitute about 60% of all chronic soft-tissue swellings affecting the hand and wrist. They usually develop spontaneously in adults aged 20 to 50, with a female: male preponderance of 3:1.People who have wear-and-tear arthritis in the finger joints closest to their fingernails are at higher risk of developing ganglion cysts near those joints. Joints or tendons that have been injured in the past are more likely to develop ganglion cysts.
TEXT 2: Diagnosing a ganglion cyst
Ganglia are evident on examination even if they cannot be seen by the naked eye. It is important that cysts are examined by a doctor because there is another type of ganglion on the dorsal wrist that occurs in people with rheumatoid arthritis. A doctor can easily differentiate between them because a rheumatoid cyst is soft and irregular in appearance. Also, a person with rheumatoid arthritis will also have proliferative rheumatoid extensor tenosynovitis.
Most ganglion cysts do not cause symptoms, but the main symptoms people experience are a noticeable swelling or lump. The lump is able to change its size, including going away completely only to return. The lump is usually soft and immobile. In some cases, the lump is painful and aching, particularly those at the base of fingers. The ache and pain is made worse by moving any nearby joints. The affected tendon may cause a sensation of muscular weakness. The back of the hands and wrists are most commonly affected.
A medical examination is generally all that is needed to confirm diagnosis but other tests could include: Aspirating some of the fluid with a syringe An ultrasound to determine if the ganglion is solid or fluid filled X-ray and/or magnetic resonance imaging may be needed if the cyst cannot be seen.
TEXT 3 Passive treatment options for a ganglion cyst
If a cyst is not causing any problems, a passive “watch and wait” approach is recommended. This means the cyst is monitored and action only taken if it increases to a point where it causes symptoms. However, even if there are no symptoms some people prefer treatment for cosmetic reasons.
Temporarily immobilising the joints around a cyst may both slow down the rate at which the cyst grows and reduce the size of the cyst. This may release the pressure on nerves, relieving pain. If a person knows what activity is the likely cause such as starting to play an instrument or using a new piece of equipment, it may be helpful to stop or modify this activity.
Simple over the counter pain relievers and/or anti-inflammatory medications may be required to alleviate pain. In some cases, modifying shoes or how they are laced can relieve the pain associated with ganglion cysts on ankles or feet.
A traditional old home remedy for a ganglion cyst consisted hitting the cyst with the Bible. Thumping a cyst with any heavy object is not recommended because the force of the blow can damage surrounding structures in the hand or foot.
TEXT 4
Another self-help approach is to try and “pop” the cyst by puncturing it with a needle. This is unlikely to be effective and can lead to infection.
Some people advocate herbal remedies that have anti-inflammatory properties such as turmeric and ginger. The true cause of ganglion cysts is not known but they are a bulge in the lining of a structure. This means it is unlikely to be part of the inflammatory process
Active treatment options for ganglion cysts.
If a cyst is causing problems, a needle aspiration performed by a qualified doctor. This simple procedure is carried out in the GP surgery or hospital outpatients department. It involves drawing the liquid contents of the cysts out of the sac via the syringe.
Needle aspiration is usually the first active treatment option offered for ganglion cysts as it is less invasive than surgery. However, nonsurgical treatment fails in about 40 to 70% of patients, necessitating surgical excision.
The cyst may be surgically removed using either open or keyhole approaches.
In open surgery the surgeon makes a medium-sized cut, usually about 5cm (2in) long, over the site of the affected joint or tendon. The sac is removed at the pedicle to reduce recurrence.
Keyhole surgery is often used if the ganglion cyst is near, or in a joint. Smaller incisions are made and a tiny camera called an arthroscope is used by the surgeon to look inside the joint and then pass instruments through the incision to remove the cyst. Excision can be done via arthroscopic or standard open surgery. Recurrence rates after surgical excision are about 5 to 15%.
Questions 1-7 For each question, 1-7, decide which text (A, B, C or D) the information comes from. You may use any letter more than once. In which text can you find information about
1 The ratio of ganglion cysts between sexes? ___________________
2 The primary dynamic way of removing ganglion cysts? ________________
3 The investigations that may be done to confirm someone has a ganglion cyst? ___________________
4 How keeping the affected area immobile for a time can reduce the effect of a ganglion cyst? _____________
5 Another type of ganglion cyst that can develop at the wrist? ____________
6 The role the bible used to play in managing ganglion cysts? _____________
7 The contents of a ganglion cyst? ___________________
Questions 8-14 Answer each of the questions, 8-14, with a word or short phrase from one of the texts. Each answer may include words, numbers or both.
8 Where ganglion cysts are usually seen? ___________________
9 What percentage of ganglion cysts come back after a surgical excision? ___________________
10 Are ganglion cysts more common in men or women? ___________________
11 What can changing shoes achieve for people with ganglion cysts in lower limbs? ___________________ 12 What are the two main complaints people with a ganglion cyst have? ___________________
13 What type of cysts develop from the fingers? ___________________
14 What is often the first invasive treatment option offered for ganglion cysts? ___________________
Questions 15-20 Complete each of the sentences, 15-20, with a word or short phrase from one of the texts. Each answer may include words, numbers or both.
15 An______________ shows if the ganglion is solid or not.
16 ___________ganglia and mucous cysts in the DIP joints account for a small number of all ganglion cysts.
17 No one really knows why ganglion cysts develop but there is a____ in the membrane around a structure 18 A surgeon can look into a ganglion cyst around a joint with an arthroscope and then_________ through an additional small cut in the skin to get rid of the cyst.
19 A ganglion cyst on a tendon on can lead to a cause a feeling of___________________ weakness.
20 Needle aspiration involves pulling the__________ of the cysts out of the sac with a needle and syringe.
PART B
TEXT 1 What Nurses Need to Know About Celiac Disease and Gluten Sensitivity
Gluten is the group name for two proteins, gliadin and glutenin, which are primarily derived from wheat, barley, rye and triticale. These proteins are responsible for the bonding of particles, giving food its shape. When gluten is consumed, those with an allergy experience an immune response which attacks the small intestine. Once the villi of the small intestine are damaged, nutrients cannot be properly absorbed. While some people may be asymptomatic throughout their lifetime, many experience at least some symptoms.
Recent research shows there is no evidence to support an increased risk of celiac disease when infants are introduced to gluten at an early age (less than 4 months). However, delayed introduction (more than 7 months) to gluten may be associated with an increased risk.
Question 1) What does the article say about the causes of celiac disease?
a) It can provoke damage to the small intestine
b) It could be linked to children’s diets
c) Normally, children don’t suffer from celiac disease
TEXT 2 Aspirin Guidelines
Aspirin should be taken with, or straight after, a meal or snack. This helps to reduce the risk of any stomach irritation. Gastro-resistant tablets (also called enteric-coated or EC tablets) can be taken before food as these have a special coating which will help to protect the stomach from irritation. Gastro-resistant tablets should be swallowed whole, they must not be crushed or chewed. If the patient is using indigestion remedies, aspirin in this form must not be taken for at least two hours before and the two hours after they are used. This is because the antacid in the remedy can affect the way the coating on these tablets works. Melt-in-the-mouth (orodispersible) tablets should be placed on the tongue and allowed to dissolve.
Question 2) What do these guidelines say about when to take aspirin?
a) Aspirin taken close to meal times can irritate the stomach lining
b) Some types of aspirin have special indications
c) It can be taken in combination with indigestion remedies
TEXT 3 Assessing the Need for a Peripheral Intravenous Cannula
Many cannulas are left in without orders for intravenous fluids or medications. Some patients end up with two, three, or even more concurrent cannulas, despite only needing one in most cases. They are often left in ‘just in case’ they might be needed. But any catheter leads directly to the bloodstream and can be a source of infection. The need for the cannula must be constantly reassessed.
When a cannula is inserted, a flashback of blood in the chamber confirms it is in the vein. Flushing the cannula with 0.9% saline before and after intravenous medications reduces admixture of medicines and decreases the risk of blockage.
Question 3) What does this article say about the use of cannulas?
a) Cannula usage should be reviewed regularly
b) In most cases, concurrent cannula use is justified
c) Cannulas can be left in place so long as they are flushed with a 0.9% saline solution
TEXT 4 Description of the ‘SecurAcath’ Device
SecurAcath’ is a single-use device to secure percutaneous catheters in position on the skin. It is intended for use in adults and children who need a central venous
catheter which is a long, thin, flexible tube that is inserted into a vein through the skin.
‘SecurAcath’ has two parts, a base and cover. The base is made up of two foldable metal legs and two securement feet. The feet are placed under the skin at the catheter insertion site and unfolded to make a subcutaneous anchor. The cover then attaches to the catheter shaft and holds it in place when it is clipped onto the base. The device stays in place as long as the catheter is needed and can be lifted off the skin to allow cleaning of the insertion site.
Question 4) How should the ‘SecurAcath’ device be used?
a) The feet can be repositioned in order to clip them to the base
b) It should be correctly assembled before attaching the cover
c) The flexible tube should be inserted into a vein first
TEXT 5 Assessment of Colorectal Polyps During Colonoscopy
Colorectal polyps are small growths on the inner lining of the colon. Polyps are not usually cancerous, most are hyperplastic polyps with a low risk of cancer. However, some (known as adenomatous polyps) will eventually turn into cancer if left untreated. Detecting and removing adenomas during colonoscopy has been shown to decrease the later development of colorectal cancers. However, removal of any polyps by polypectomy may have adverse effects such as bleeding and perforation of the bowel.
It can take three weeks for a person to get the examination results for polyps that were removed during colonoscopy, and they may feel anxious during this waiting period. Using virtual chromoendoscopy technologies may allow real-time differentiation of adenomas and hyperplastic colorectal polyps during colonoscopy, which could lead to quicker results. Question
5) What does the article tell us about colonoscopies?
a) Colonoscopy and polypectomy procedures are thought to be risk-free
b) Virtual chromoendoscopy technology could speed up the process
c) Most hyperplastic polyps become cancerous if left untreated
TEXT 6 Osteomyelitis After Traumatic Knee Injury
A 56-year-old woman was admitted to a hospital for the treatment of osteomyelitis following a traumatic knee injury. She received the antibiotic Gentamicin in accordance with the hospital’s usual protocol. Kinetics, blood drug levels, and renal function were monitored, and dosage recommendations were made. However, a permanent vestibulopathy (or balance disorder) resulted from the antibiotic.
During the case investigation, the patient testified that she experienced “roaring” in her ears while hospitalized. (The roaring is a form of tinnitus) She further testified that she was not ambulatory; she was restricted to bed rest. No staff member inquired about unusual ear symptoms or told her to report such symptoms. Consequently, a lawsuit was brought against the hospital, specifically against the pharmacists.
Question 6) What went wrong in the treatment of the 56-year-old woman?
a) The woman was infected by vestibulopathy while in hospital
b) The correct dosage was not balanced
c) Staff members failed to take note of the woman’s symptoms
PART C TEXT 1
Many adult hospital inpatients need intravenous (IV) fluid therapy to prevent or correct problems with their fluid and/or electrolyte status. Deciding on the optimal amount and composition of IV fluids to be administered and the best rate at which to give them can be a difficult and complex task, and decisions must be based on careful assessment of the patient’s individual needs.
Errors in prescribing IV fluids and electrolytes are particularly likely in emergency departments, acute admission units, and general medical and surgical wards rather than in operating theatres and critical care units. Surveys have shown that many staff who prescribe IV fluids know neither the likely fluid and electrolyte needs of individual patients, nor the specific composition of the many choices of IV fluids available to them. Standards of recording and monitoring IV fluid and electrolyte therapy may also be poor in these settings. IV fluid management in hospital is often delegated to the most junior medical staff who frequently lack the relevant experience and may have received little or no specific training on the subject.
The ‘National Confidential Enquiry into Perioperative Deaths’ report in 1999 highlighted that a significant number of hospitalised patients were dying as a result of infusion of too much or too little fluid. The report recommended that fluid prescribing should be given the same status as drug prescribing. Although mismanagement of fluid therapy is rarely reported as being responsible for patient harm, it is likely that as many as one in five patients on IV fluids and electrolytes suffer complications or morbidity due to their inappropriate administration.
There is also considerable debate about the best IV fluids to use (particularly for more seriously ill or injured patients), resulting in wide variation in clinical practice. Many reasons underlie the ongoing debate, but most revolve around difficulties in interpretation of both trial evidence and clinical experience. For example, many accepted practices of IV fluid prescribing were developed for historical reasons rather than through clinical trials. Trials cannot easily be included in meta-analyses because they examine varied outcome measures in heterogeneous groups, comparing not only different types of fluid with different electrolyte content, but also different volumes and rates of administration. In addition, most trials have been undertaken in operating theatres and critical care units rather than admission units or general and elderly care settings. Hence, there is a clear need for guidance on IV fluid therapy for general areas of hospital practice, covering both the prescription and monitoring of IV fluid and electrolyte therapy, and the training and educational needs of all hospital staff involved in IV fluid management.
The aim of these guidelines is to help prescribers understand the physiological principles that underpin fluid prescribing the pathophysiological changes that affect fluid balance in disease states and the indications for IV fluid therapy. In developing the guidelines, it was necessary to limit the scope by excluding patient groups with more specialised fluid prescribing needs. It is important to emphasise that the recommendations do not apply to patients under 16 years, pregnant women, and those with severe liver or renal disease, diabetes or burns. They also do not apply to patients needing inotropes and those on intensive monitoring, and so they have less relevance to intensive care settings and patients during surgical anaesthesia. Patients with traumatic brain injury (including patients needing neurosurgery) are also excluded. The scope of the guidelines does not cover the practical aspects of administration (as opposed to the prescription) of IV fluids. It is hoped that these guidelines will lead to better fluid prescribing in hospitalised patients, reduce morbidity and mortality, and lead to better patient outcomes.
The guidelines will assume that prescribers will use a drug’s summary of product characteristics to inform decisions made with individual patients. All patients continuing to receive IV fluids need regular monitoring. This should initially include at least daily reassessments of clinical fluid status, laboratory values (urea, creatinine and electrolytes) and fluid balance charts, along with weight measurement twice weekly. It is important to remember that patients receiving IV fluid therapy to address replacement or redistribution problems may need more frequent monitoring. Additional monitoring of urinary sodium may be helpful in patients with high-volume gastrointestinal losses. Patients on longer-term IV fluid therapy whose condition is stable may be monitored less frequently, although decisions to reduce monitoring frequency should be detailed in their IV fluid management plan. Clear incidents of fluid mismanagement (for example, unnecessarily prolonged dehydration or inadvertent fluid overload due to IV fluid therapy) should be reported through standard critical incident reporting to encourage improved training and practice (see Consequences of fluid mismanagement to be reported as critical incidents).
Questions 7-14
7) What does the first paragraph tell us about intravenous (IV) fluid therapy?
a) Most patients receive a standard composition of fluids
b) Electrolyte status should be kept at the optimal level
c) It is not easy to decide on the correct volume and speed of delivery of fluids
d) It is difficult to correct problems
8) What have surveys shown about intravenous (IV) fluid therapy?
a) There is often a lack of information about correct dosage
b) Sometimes, staff mixed up electrolyte fluids with standard IV fluids
c) Intravenous (IV) fluid therapy should be delegated to junior medical staff
d) Mistakes made in operating theatres were often fatal
9) What did the 1999 report highlight?
a) A small number of patients died because they were prescribed the wrong medication
b) Around 20% of patients experience problems due to incorrect IV fluid therapy
c) Some hospitals fail to report deaths due to mismanaged procedures
d) Not all Perioperative deaths could be linked to IV fluid therapy
10) What does the fourth paragraph tell us about IV fluid therapy?
a) Seriously ill patients generally need more fluids that injured patients
b) There are historical reasons to prolong the use of IV fluid therapy
c) The best IV fluids are more expensive
d) Not everyone agrees on the most suitable fluids to use
11) Why is it difficult to perform meta-analyses of trials?
a) There are not enough qualified analysts
b) Trials usually don’t take place in different healthcare settings
c) The volume of data is too great to analyse
d) More hospital staff need training before the trials take place
12) What do we learn about the scope of the guidelines in the fifth paragraph?
a) The guidelines are not appropriate for all types of patients
b) Patients needing inotropes and those on intensive monitoring were included for historical reasons
c) Pathophysiological patients were excluded because they cannot be given IV fluid therapy
d) The guidelines only apply to men (that is to say, adult male patients)
13) According the sixth paragraph, how often should clinical fluid status be reassessed?
a) Twice a day or more frequently
b) Once every 24 hours
c) Twice a week
d) Never – routine reassessment can be monitored by machine
14) What should be done in the case of fluid mismanagement?
a) Additional monitoring should be carried out
b) Rehydration should be prolonged
c) Information about occurrences should be conveyed to the appropriate authorities
d) The person or persons involved should be criticised
PART C TEXT 2
A CT scan is a specialised X-ray test. It can give quite clear pictures of the inside of your body. In particular, it can give good pictures of soft tissues of the body which do not show on ordinary X-ray pictures. CT stands for computerised tomography. It is sometimes called a CAT scan. CAT stands for Computerised Axial Tomography. The CT scanner looks like a giant thick ring. Within the wall of the scanner there is an X-ray source. Opposite the X-ray source, on the other side of the ring, are X-ray detectors. You lie on a couch which slides into the centre of the ring until the part of the body to be scanned is within the ring. The X-ray machine within the ring rotates around your body. As it rotates around, the X-ray machine emits thin beams of X-rays through your body, which are detected by the X-ray detectors.
The detectors detect the strength of the X-ray beam that has passed through your body. The denser the tissue, the less X-rays pass through. The X-ray detectors feed this information into a computer. Different types of tissue with different densities show up as a picture on the computer monitor, in different colours or shades of grey. So, in effect, a picture is created by the computer of a slice (cross-section) of a thin section of your body.
As the couch moves slowly through the ring, the X-ray beam passes through the next section of your body. So, several cross-sectional pictures of the part of your body being investigated are made by the computer. Newer scanners can even produce 3-dimensional pictures from the data received from the various slices of
the part of the body being scanned.
A CT scan can be performed on any section of the head or body. It can give clear pictures of bones. It also gives clear pictures of soft tissues, which an ordinary X-ray test cannot show, such as muscles, organs, large blood vessels, the brain and nerves. The most commonly performed CT scan is of the brain to determine the cause of a stroke, or to assess serious head injuries.
Usually, very little preparation is necessary. It depends on which part of your body is to be scanned. You will be given instructions by the CT department according to the scan to be done. As a general rule, you will need to remove any metal objects from your body, such as jewellery, hair clips, etc. It is best not to wear clothes with metal zips or studs. You may be asked not to eat or drink for a few hours before your scan, depending on the part of your body to be scanned.
The CT scan itself is painless. You cannot see or feel X-rays. You will be asked to stay as still as possible, as otherwise the scan pictures may be blurred. Conventional CT scans can take between 5-30 minutes, depending on which part of the body is being scanned. More modern CT scans (helical CT scans) take less than a minute and also use less radiation.
As the scan uses X-rays, other people should not be in the same room. The operator controls the movement of the couch and scanner from behind a screen or in a separate control room so that they are protected from repeated exposure to X-rays. However, communication is usually possible via an intercom, and you will be observed at all times on a monitor. Some people feel a little anxious or claustrophobic in the scanner room when they are on their own. You can return to your normal activities as soon as the scan is over. The pictures from the scan are studied by an X-ray doctor (radiologist) who sends a report to the doctor who requested the scan.
CT scans use X-rays, which are a type of radiation. Exposure to large doses of radiation is linked to developing cancer or leukaemia – often many years later. The dose of X-ray radiation needed for a CT scan is much more than for a single X-ray picture but is still generally quite a low dose. The risk of harm from the dose of radiation used in CT scanning is thought to be very small but it is not totally without risk. As a rule, the higher the dose of radiation, the greater the risk. So, for example, the larger the part of the body scanned, the greater the radiation dose. And, repeat CT scans over time cause an overall increase of dose. Various studies have aimed to estimate the risk of developing cancer or leukaemia following a CT scan. In general, the risk is small. In many situations, the benefit of a CT scan greatly outweighs the risk.
Questions 15-22
15) What advantage does a CT scan give over a standard X-ray?
a) It emits less radiation
b) It can take pictures of bones and soft tissues
c) It is quieter and uses less electricity
d) The patient can lie down during the scan
16) What can be seen on a CT scan result?
a) Tissue thicknesses and densities can be shown using different colours
b) The computer displays the date, time and patient’s name on the result
c) When this article was written, CT scans could only show shades of grey on the results
d) Cross-dimensional attributes are shown on the results in colour or shades of grey
17) What does the third paragraph tell us about the CT scans?
a) Usually, more than one picture is obtained
b) 3-dimensional pictures provide more information that standard cross-sectional pictures
c) The CT ring can be programmed to move the coach slowly
d) Images and scans can be stored on computers for up to a year
18) What type of scan is carried out most frequently?
a) Scans of the head and neck b) Scans of the chest and upper body
c) Whole body scans
d) Scans of the head only
19) What should you wear for your CT scan?
a) Clothing that is free of any metal
b) A standard hospital gown
c) There are usually no restrictions on clothing
d) Some scans require an absence of clothing
20) What can influence the clarity of CT images?
a) Temperature
b) Movement
c) Radiation levels
d) Levels of pain or discomfort
21) What does the article say about the number of people in the CT room?
a) A Only the operator will be with you in the CT room
b) You can ask for one or two people to stay with you during the scan
c) You can only be accompanied if you feel anxious or claustrophobic
d) You will be alone in the CT room
22) What does the last paragraph say about the levels of risk?
a) Generally, the risks are not as significant as the potential advantages
b) Some people have developed cancer or leukaemia after a CT scan
c) CT scanners pose a lower risk than standard X-ray machines
d) There is a high risk of cancer if you have a large body
Free admission and English Courses. കാശ് കൊടുക്കാതെ അഡ്മിഷൻ. FREE ഇഗ്ലീഷ് കോഴ്സുകൾ. ഈ ഓഫർ നേടൂ. Contact us at +91 9886926773 പ്രോസസ്സിംഗ് ആയാസകരം.

New batch is open. Join today!
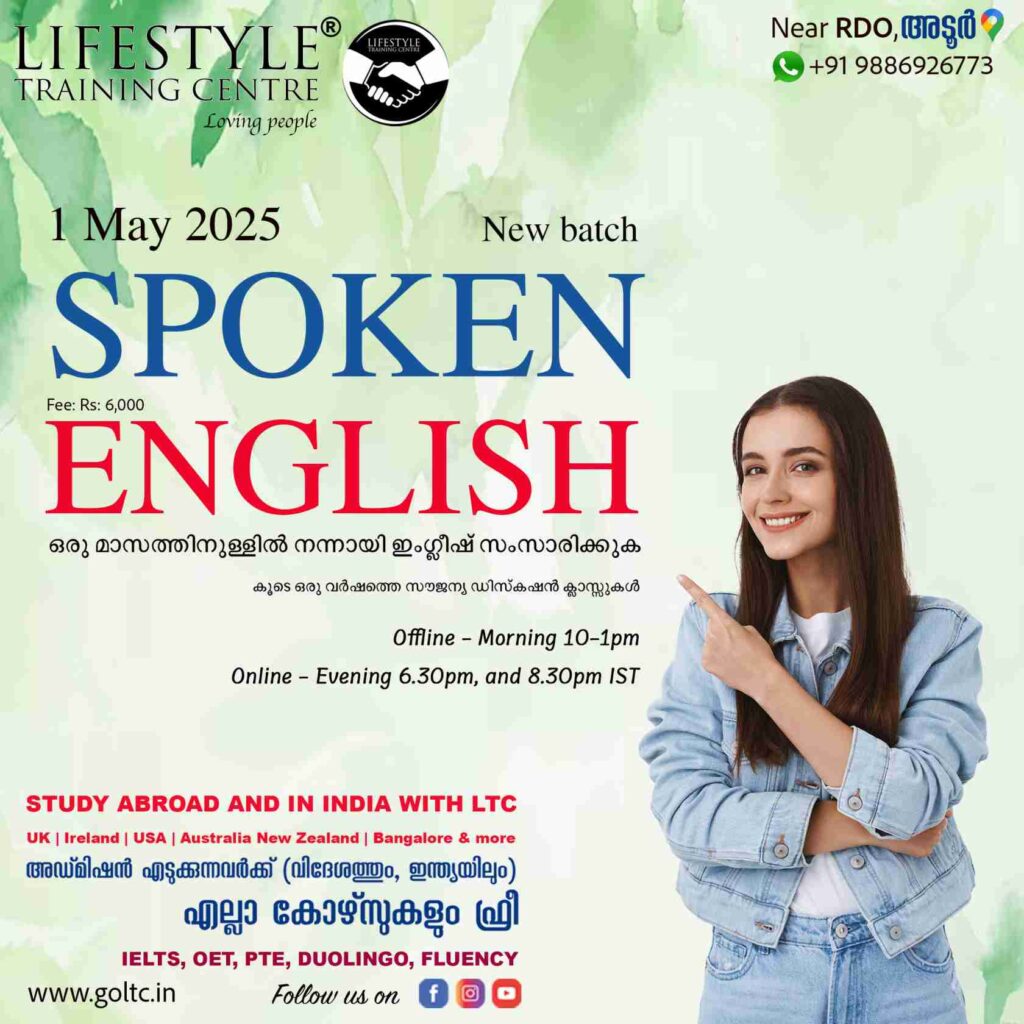
Ready to study abroad or master OET, PTE, IELTS, Duolingo, Phonetics, or Spoken English?
📞 Call us now at +91 9886926773
📱 Call/WhatsApp/Text: +91 9886926773
📧 Email: mail@goltc.in
Visit us in person by following the directions on Google Maps. We look forward to welcoming you to the Lifestyle Training Centre.
Follow Lifestyle Training Centre on social media:
Thank you very much!
Would you like to download a copy of the practice test? Please click on the download button below:

