Text A Anaphylactic shock occurs rapidly and is life-threatening. Anaphylactic shock is a systemic, type I hypersensitivity reaction that often has fatal consequences. Anaphylaxis causes the immune system to release a flood of chemicals that can cause a person to go into shock.
Text B Pathophysiology: Anaphylaxis occurs in an individual after re exposure to an antigen to which that person has produced a specific lgE antibody.
Re exposure: Upon re exposure to the sensitized allergen, the allergen may cross-link the mast cell or basophil surface-bound allergen-specific IgE resulting in cellular degranulation as well as de novo synthesis of mediators.
Binding: Immunoglobulin E (IgE) binds to the antigen (the foreign material that provokes the allergic reaction).
Activation: Antigen-bound IgE then activates FcεRI receptors on mast cells and basophils.
Inflammatory mediators release. This leads to the release of inflammatory mediators such as histamine.
Histamine release: Many of the signs and symptoms of anaphylaxis are attributable to binding of histamine to its receptors; binding to H1 receptors mediates pruritus, rhinorrhea, tachycardia, and bronchospasm.
Prostaglandin D2: Prostaglandin D2 mediates bronchospasm and vascular dilatation,principle manifestations of anaphylaxis.
Leukotriene C4: Leukotriene C4 is converted into LTD4 and LTE4, mediators of hypotension, bronchospasm, and mucous secretion during anaphylaxis in addition to acting as chemotactic signals for eosinophils and neutrophils.
Causes Allergy symptoms aren’t usually life-threatening, but a severe allergic reaction can lead to anaphylaxis.
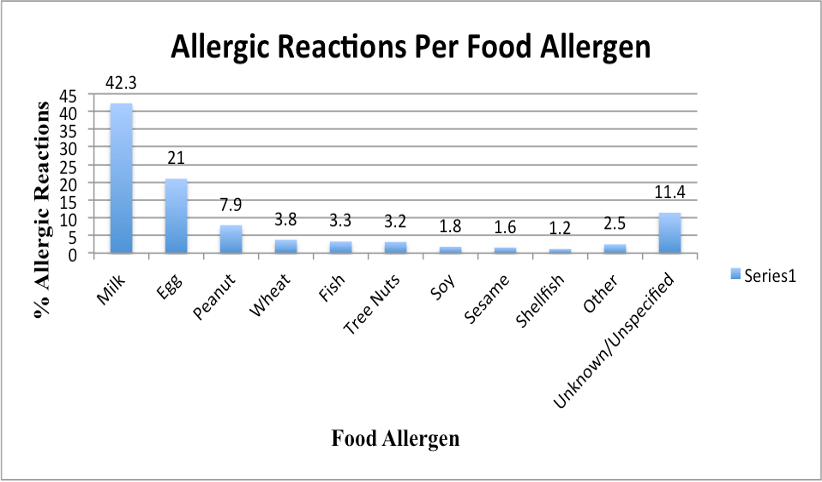
Food allergies: The most common anaphylaxis triggers in children are food allergies, such as to peanuts, and tree nuts, fish, shellfish and milk.
Medication allergies: Certain medications, including antibiotics, aspirin and other over-the-counter pain relievers, and the intravenous (IV) contrast used in some imaging tests.
Insect allergies: Stings from bees, yellow jackets, wasps, hornets and fire ants.
Latex allergy: Latex allergy develops after many previous exposures to latex.
Clinical Manifestations: An anaphylactic reaction produces the following symptoms:
Anxiety: The first symptoms usually include a feeling of impending doom or fright.
Skin reactions: Skin reactions such as hives, itching, and flushed or pale skin follow.
Shortness of breath: Constriction of the airways and a swollen tongue or throat could cause wheezing and troubled breathing.
Hypotension: A low blood pressure occurs as one of the major symptoms of shock.
Tachycardia: The heart compensates through pumping faster and trying to deliver blood to all body systems.
Dizziness: The patient may feel dizzy which could lead to fainting.
Medical Management: Treatment of anaphylactic shock include:
Remove antigen: Removing the causative antigen such as discontinuing an antibiotic agent could stop the progression of shock.
Administer medications: Administer medications that restore vascular tone and provide emergency support of basic life functions.
Cardiopulmonary resuscitation: If cardiac arrest and respiratory arrest are imminent or have occurred, cardiopulmonary resuscitation is performed.
Endotracheal intubation: Endotracheal intubation or tracheostomy may be necessary to establish an airway.
Intravenous therapy: IV lines are inserted to provide access for administering fluids
Text C
Text D Quick reference anaphylaxis algorithm. Rapid assessment:
Airway: look for and relieve airway obstruction; call for help early if there are signs of obstruction. Remove any traces of allergen remaining (eg, nut fragments caught in teeth, with a mouthwash; bee stings without compressing any attached venom sacs).
Breathing: look for and treat bronchospasm and signs of respiratory distress.
Circulation: colour, pulse and BP.
Disability: assess whether responding or unconscious.
Exposure: assess skin with adequate exposure, but avoid excess heat loss.
Consider anaphylaxis when there is compatible history of rapid-onset severe allergic-type reaction with respiratory difficulty and/or hypotension, especially if there are skin changes present.
Give high-flow oxygen – using a mask with an oxygen reservoir (greater than 10 litres min-1 to prevent reservoir collapse). Lay the patient flat: Raise the legs (with care, as this may worsen any breathing problems).
In pregnant patients, use a left lateral tilt of at least 15° (to avoid caval compression).
Adrenaline (epinephrine) intramuscularly (IM) in the anterolateral aspect of the middle third of the thigh (safe, easy, effective):
1. Food allergy may cause anaphylactic shock ……………………….
2. History of previous exposure leads to anaphylaxis in persons with repeated exposure to the same antigen ……………………….
3. Individuals may feel itching after the exposure ………………………….
4. One fifth of the allergic reactions is due to egg ……………………
5. Immediate action to be taken when a person goes into anaphylactic shock ……………………….
6. Anaphylactic shock may also cause death ……………………….
7. H1 receptors may cause breathing difficulty ……………………….
Questions 8-14. Answer each of the questions, 8-4, with a word or short phrase from one of the texts. Each answer may include words, number of the both. Your answers should be correctly spelled.
8. What should be given in order to maintain respiration? ……………………
9. What can be avoided by removing the antigen from the body? …………………
10. What is released by the immune system during anaphylaxis? ……………………………….
11. What is the most common cause of anaphylaxis in children? ………………
12. Which allergy may occur after several previous exposures? …………………….
13. Which position is given to pregnant women in order to maintain breathing? ………..
14. What should be checked to assess circulation?……….
Questions 15-20. Complete each of the sentences, 15- 20, with a word or short phrase from one of the texts. Each answer may include words, number or both. Your answers should be correctly spelled
15. Anaphylactic shock is a ………………….type 1 systemic reaction.
16. One of the major symptoms of shock is…….
17. …………………. is given intramuscularly to stop progression of shock.
18. …………….. symptoms usually do not cause fatal consequences.
19. ………………….activates FcέRI receptors on mast cells and basophils.
20. Medications to be administered to restore………. and provide emergency support.
Free admission and English Courses. കാശ് കൊടുക്കാതെ അഡ്മിഷൻ. FREE ഇഗ്ലീഷ് കോഴ്സുകൾ. ഈ ഓഫർ നേടൂ. Contact us at +91 9886926773 പ്രോസസ്സിംഗ് ആയാസകരം.

New batch is open. Join today!

Ready to study abroad or master OET, PTE, IELTS, Duolingo, Phonetics, or Spoken English?
📞 Call us now at +91 9886926773
📱 Call/WhatsApp/Text: +91 9886926773
📧 Email: mail@goltc.in
Visit us in person by following the directions on Google Maps. We look forward to welcoming you to the Lifestyle Training Centre.
Follow Lifestyle Training Centre on social media:
Thank you very much!
Would you like to download a copy of the practice test? Please click on the download button below:


Pingback: ANAPHYLACTIC SHOCK OET READING | Lifestyle Training Centre®
Pingback: ANAPHYLACTIC SHOCK OET READING ANSWERS | Lifestyle Training Centre®