MR JOHN McINTYRE – 68 year old
Born: 1941
This 68 year old married man has been getting monitored at the Community Health Centre, Richmond. He and his wife are moving to The Lake Retirement Village Bannockburn
11/2001 – First attended Community Health Centre, Richmond
10/2009 – Last attended the Centre
DIAGNOSIS: Hypertension, Congestive cardiac failure, Chronic obstructive airways disease (COAD)
SOCIAL HISTORY: Married, Three children; one grandchild, Lives in own home with his wife
Wife has no control over his lifestyle or medication. He resents his children’s advice about the need to change his lifestyle. Now moving to a self-contained Unit at The Lake Retirement Village (Anticipate this will happen in one week’s time). Apart from a small amount of savings, Mr. and Mrs. McIntyre plan to live on the Aged Pension. Has been excessively drinking alcohol for past 30 years. Has been excessively smoking (40/day) for the past 35 years. Claims he will stop smoking once he moves to the new Unit. He will try and cut down on the drinking
NURSING MANAGEMENT AND PROGRESS
Medications include diuretics, antihypertensive, vasodilators and bronthodilators
Has received regular monitoring by Community Nurse to achieve medication compliance
Further details in patient’s personal casebook (with the patient)
DISCHARGE PLAN: Establish contact with a sympathetic medical practitioner
Monitor medication compliance and diet, Encourage patient to stop smoking
Encourage patient to stop drinking, Encourage patient to take moderate regular exercise
WRITING TASK: Mr. McIntyre needs to be monitored by a sympathetic GP so that his present regime continues in his new home. Using the information in the above case notes, write a letter referring the patient into the care of Dr Joan Meagher, General Practitioner, Bannockburn Community Health Centre, 2 Pope Street Bannockburn Victoria 3331. You must use full sentences in your letter – not notes / bullet points. Write no more than 25 lines about 180 to 200 words.
Submit your OET letters for correction: (for a minimal fee)
https://goltc.in/oet-writing-correction/
Free admission and English Courses. കാശ് കൊടുക്കാതെ അഡ്മിഷൻ. FREE ഇഗ്ലീഷ് കോഴ്സുകൾ. ഈ ഓഫർ നേടൂ. Contact us at +91 9886926773 പ്രോസസ്സിംഗ് ആയാസകരം.

New batch is open. Join today!
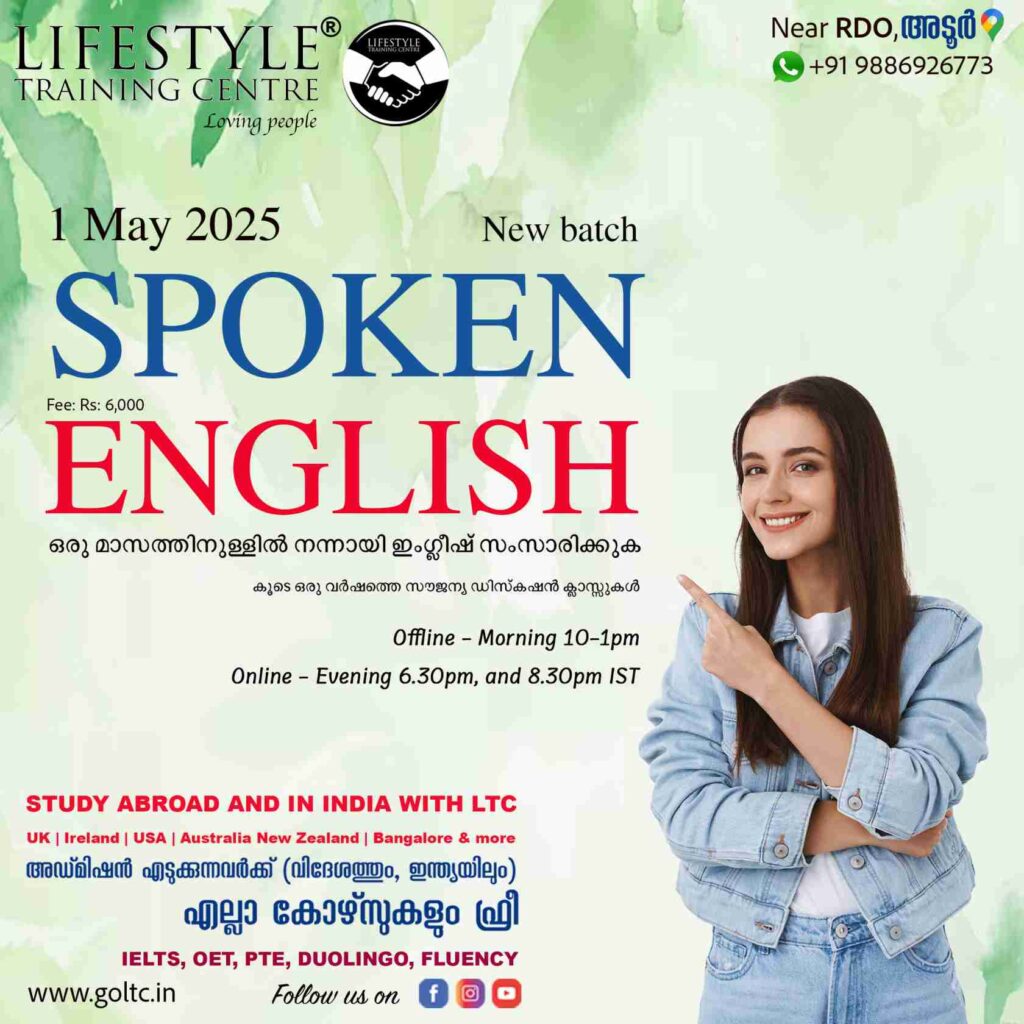
Ready to study abroad or master OET, PTE, IELTS, Duolingo, Phonetics, or Spoken English?
📞 Call us now at +91 9886926773
📱 Call/WhatsApp/Text: +91 9886926773
📧 Email: mail@goltc.in
Visit us in person by following the directions on Google Maps. We look forward to welcoming you to the Lifestyle Training Centre.
Follow Lifestyle Training Centre on social media:
Thank you very much!

Submit your OET letters for correction: (for a minimal fee)
https://goltc.in/oet-writing-correction/
Hi Jomon,
This is Writing Task 48 can you please correct it:
27/07/1992
Mrs. Hoa Tran
Romand Council
Dear Mrs. Tran,
Re: Mrs. Guy Hoang Chung, DOB: 17/05/1953
Thank you for seeing Mrs.Chung, a 40 years old house wife who recently had a caesarean delivery. I am referring her to you to help communicate with her and understand the reasons of her depression.
On 10/07/1992, Mrs. Chung had a caesarean delivery due to outlet insufficency and non-reassuring contractions. 10 days after the delivery, the neonate was in good health and sutures were removed from Mr. Chuang and she was discharged.
Mrs. Chung’s husband is busy with his work as a business importer, and her 3 children are busy with school and studies and there seems to be no one available to support Mrs. Chung in caring for her newborn, which is overwhelming her. I was reffered to home visit Mrs. Chung today by the maternity hospital to follow-up with her, but there seems to ba a language barrier between us, since she can’t speak English. She also doesn’t leave her bed and refuses any medical intervention.
Kindly communicate with Mrs. Chung to interpret her concerns, explaining to her the reasons of the home visit, and to come up with a management plan for the resolution of her symptoms. Please feel free to contact me for any inquiries.
Regards,
Registered Nurse
Thank you for seeing Mrs.Chung, a 40 years old house wife(,) who recently had a caesarean delivery. I am referring her to you to help communicate with her and understand the reasons of her depression.
On 10/07/1992, Mrs. Chung had a caesarean delivery due to outlet insufficency (insufficiency) and non-reassuring contractions. 10 days after the delivery, the neonate was in good health and sutures were removed from Mr. Chuang (,) and she was discharged.
Mrs. Chung’s husband is busy with his work as a business importer, and her 3 children are busy with school and studies (start a new sentence) and (There)there seems to be no one available to support Mrs. Chung in caring for her newborn, which is overwhelming her. I was reffered (referred) to home visit (home-visit)Mrs. Chung today by the maternity hospital to follow-up with her, but there seems to ba (be) a language barrier between us, since she can’t speak English. She also doesn’t leave her bed and refuses any medical intervention.
Kindly communicate with Mrs. Chung to interpret her concerns, explaining to her the reasons of (for) the home visit, and to come up with a management plan for the resolution of her symptoms. Please feel free to contact me for any inquiries.
Regards, (Yours faithfully, – as the name of the recipient is given – if not, Yours sincerely, )
Registered Nurse
Your writing is good. However, the arrangement of the letter can be improved. Social history is important here. Kindly go through a model I’ve written:
https://goltc.in/guy-hoang-chung-oet-letter/
You could see in my version that I have clearly explained to the recipient the possible reasons for the patient’s depression. You need to understand the real concern before you write. Hope this helps.
Thank you very much JOMON for looking into it. Can you please see my writing in TASK 59 as well, with a marking it if possible. Thanks in advance.
14/04/2018
Emergency Doctor on Duty
NewtownHospital
Comer Street
Newtown 1104
Dear Emergency Doctor,
Re: Ms. Patricia Styles, DOB: 04/08/1955
Thank you for seeing Ms. Styles, a 63 years old patient, who was recently admitted for pericarditis. I am referring her to you for urgent medical assessment and treatment of her relapsing percarditis.
On 07/04/2018, Ms. Styles was complainig of chest pain, shortness of breath, and fatigue. Her blood test showed elevated ESR and creatnine. Throat swab was positive for Type B Influenza and echocardiogram confirmed pericarditis. Ms. Styles was treated with IV antibiotics and saline and was discharged on 09/04/2018 with home-visit follow-up.
Ms. Styles has a history of hypertension, diabetes mellitus, and depression, that is treated with Carpinol, Metformin + Glipizide, and medical councils, respectively. Her husband died 3 years ago, and she manages her chores independently, with occassional help of her cousin with medications.
Ms. Styles had her first home-visit on 12/04/2018 which showed no abnormalities. However, today’s home-visit shows fever, shortness of breath, increased HR of 122, RR of 28, and BP of 180/90, which is concerning for a relapse of her condition.
Based on what is indicated above, please perform an urgent workup for Ms. Styles with providing the appropriate management for her pericarditis. Feel free to contact me for any inquiries.
Yours Sincerely,
Registered Nurse
word count: 220 words
Dear Emergency Doctor,
Re: Ms. Patricia Styles, DOB: 04/08/1955
1st paragraph is good. However, I recommend you to do the opposite way. Referral first, and then talk about the diagnosis. This will make your writing easy every time.
Eg: I am writing to refer Ms Styles who requires urgent medical assessment and care. She has been undergoing treatment in our facility for complications associated with pericarditis. (No need to mention age as DOB is given already)
Thank you for seeing Ms. Styles, a 63 years old patient, who was recently admitted for pericarditis. I am referring her to you for urgent medical assessment and treatment of her relapsing percarditis.
On 07/04/2018, Ms. Styles was complainig of chest pain, shortness of breath, and fatigue. Her blood test showed elevated ESR and creatnine.
(Always include subject in OET writing – If not, it will be become note form) (eg: Her throat swab) Throat swab was positive for Type B Influenza and echocardiogram confirmed pericarditis. Ms. Styles was treated with IV antibiotics and saline and was discharged on 09/04/2018 with home-visit follow-up.
Ms. Styles has a history of hypertension, diabetes mellitus, and depression, that is treated with Carpinol, Metformin + Glipizide, and medical coun-cils, respectively. Her husband died 3 years ago, and she manages her chores independently, with occasional help of her cousin with medications.
(this paragraph should go up and the social history down in order to ensure flow) Ms. Styles had her first home-visit on 12/04/2018 which showed no abnormalities. However, today’s home-visit shows (use passive- during the home-visit today, it was found out that) fever, shortness of breath, increased HR of 122, RR of 28, and BP of 180/90, which is concerning for a relapse of her condition.
Based on what is indicated above, please perform an urgent workup for Ms. Styles with providing the appropriate management for her pericarditis.
Feel free to contact me for any inquiries.
Yours Sincerely, (small letter sincerely)
Registered Nurse
word count: 220 words
The letter is good. However, there is place for improvement. Check use of possessive noun, passive formation, avoid note form, paragraph order, DOB, Capitalisation. Good job.
Thank you very much Mr. Jomon. I really appreciate your help and advice. My exam is coming soon and I wanted to your help (if you don’t mind) in correcting some of my writing tasks, since writing is my weakest part of the exam.
22/06/2011
Renal Clinical Nurse Specialist (CNS)
Bunbury Community Health Centre
Dear Renal CNS,
Re: Mr. Dallas Walters, Aged 51.
I am writing to refer Mr. Walters for the continued care of his condition at the health centre. Mr. Walters has Chronic Renal Failure, that has been managed recently with continuous ambulatory peritoneal dialysis (CAPD).
On 16/06/2011, Mr. Walters was admitted to our hospital after detoriation of his renal failure, which was diagnosed since 4 years. CAPD catheter was inserted successfully, but he needed continued cardiac assessment due to signs of hyperkalemia, eventhough he had serum K+ of 4. Mr. Walters also had a prolonged hospital stay due to acute psychosis, and delayed understanding of Mr. Walters and his wife on how to use CAPD.
Mr. Walters was discharged today. He has a history of schizophrenia, for which he has a Disability Support Pension, and Diabetes Mellitus, for which he had a catract removal surgery in the left eye due to retinopathy. He also has long history of smoking and drinking, which he quitted for 4 years.
Kindly monitor the catheter for signs of infection or pertonitis, educate him to decrase K+ dietary intake, and observe for any signs of psychosis. If needed, please provide a health worker for CAPD use education. Contact me for any inquiries.
Yours sincerely,
Registered Nurse
Word count: 220 words
Hi JOMON,
please help me in correcting my writing tasks as my exam will be next week and I am worried. It has been a while since I have sent you the previous comment and you did not reply to me.
I hope to hear your reply soon.
Regards,
Omar
Your writing is good. You could improve in the following areas:
1. Info about discharged can be written at first, rather than later: Mr X requires continuity of care and management, following his discharged today.
2. Past form of quit is quit- not quitted.
3. A history – no – He has history.
4. Use since and for correctly. Use correct tenses. Eg: He also has long history of smoking and drinking, which …. : Just write. He has not been smoking or drinking alcohol for the past four years.
4. Ending. If you have further queries, please do not hesitate to contact me.
5. Avoid note form. Every sentence should have subject and verb.
Thank you once more Jomon for correcting like always. Can you please correct Task 4,7,9. I tried to follow your instructions and minimize my errors.
TASK 4:
18/04/2008
Dr Austin Williams
Western Medical Centre
1150 Footscary Road
Sunshine, Victoria 3011
Dear Dr. Williams,
Re: Mr Henry Mcdonald, DOB: 23/06/1946
I am writing you to refer Mr Mcdonald to your medical centre, for continued care and monitoring of his condition.
On 16/04/2008, Mr Mcdonald was admitted to our hospital for management of right-side hemiplegia. He had transient left vision loss, weakness of right arm, and dribbling salaiva with aphasia. On doppler ultrasound, 50% stenosis of right carotid artery and complete stenosis on the left was visiualised. CT scan of the brain showed no abnormalities.
He is being managed with dipyridamole, a 1000 calorie/day diet, and lip/mouth exercises. Mr Mcdonald has a history of myocardial infarction 5 years ago, and hypercholestremia trated with aspirin. Moreover, he has a weight of 115kg and lifes with his partner. Mr Mcdonald partner is concerned due to his depression one month since his symptoms.
Based on what is indicated above, please advice Mr Mcdonald to cut-off smoking, and follow-up with him for a month period. He might need anticoagulation or surgery depending on his symptoms. If the aphasia persists please refer to a speech specialist or GP. He will also require a psychiatrist for addressing his depression, or give anti-depressant if needed.
Please contact me for any inquiries.
Yours sincerely,
Charge Nurse
TASK 7:
11/11/2008
Mrs. Tom Wisdom
23 Wellman St.
Camberwell 330
Dear Mrs. Wisdom,
Re: Kim Morley, Aged 36
Thank you for seeing Morley. I am referring Kim for the care and management of his sleep apnoea.
On 10/11/2008, Morley was admitted for Mino RTA after sleeping while driving. Morley polysmnography study confirmed obstructive sleep apnoea (OSA). Morley was claustrophopic to face mask, so nasal trumpets was used instead. Morley EEG, EOG, and EKG were recorded with ambien given for testing.
Today, morley is discharged with a plan of avoiding any narcotics, hypnotics, or sedatives. In addition, avoide any heavy work and driving until apnoea is treated. Morley will be referred to a dietitian for weight-loss program.
Morley is also adviced to use heated humidifier and nasal decongestant. Morley is given info about quit program for smoking, alchol, and caffiene.
Morley has a history of loud snoring, depression and obesity of 150kg. Despite several attempts for weight-loss nothing was successful. Moreover, Morley suffered from gout and psoriasis 2 years ago, had malaria on 1998, and appendectomy on1990. Morley intakes 3-4 glasses of wine and caffiene daily, and smokes a pack/day. Morley is divorced with 2 children and owns a business.
Kindly, provide morley with CPAP machine, with indications on how to use. Please contact me for any inquiries.
Yours sincerely,
Charge Nurse
TASK 9:
Admission Officer
Torquay Nursing Home
77 Jan Juc
St Torquay 3763
Dear Admission Officer,
Re: Mrs Victoria Flangan, Aged 88
I am writing you to refer Mrs. Flangan to your nursing home, for the continued care and support of her mental status.
On 16/02/2008, Mrs Flangan was admitted due to confusion, aggression, and paranoid behaviour. She was diagnosed with psychotic features related to parkinson medication side-effects. Her medication was changed from Levodopa/Carbidopa 100/25 qid, to 1.25mg Bromoryptpine mesylate/night for her first week, then 1-2.5mg/night in her second week, and now 1.9mg/night.
Mr. Flangan was also provided physical therapy, and exercises for speaking and swallowing. On discharge, her mental status issues has improved by medication changes, but her dementia and disorientation persists. She ambulates with a stick, and wears both glasses and hearing aids.
Mrs Flangan lives indpendently with her husband and has 2 children. Her husband finds diffculty in dealing with her aggressive behaviour. She feels disoriented when waking to work or gardening.
Kindly, prepare food for her that is easily swallowed and chewed. In addition, continue her physiotherapy and her speaking/swallowing exercises. Provide elevated toilet seats, upright chair with arms, and elevated slip on shoes. Please avoid any rugs to avoid fallings.
Please contact me for any concerns.
Yours faithfully,
Hi,
– Remove comma before for
– Advice is noun. Use Advise for verb
_Your letters have note forms.. Use subject and verb.- include names. Mammography confirmed xyz – instead write – Her mammography confirmed xyz.
Apart from these issues, your letters are fine and well constructed.
Thank you for your reply and teachings, JOMON!